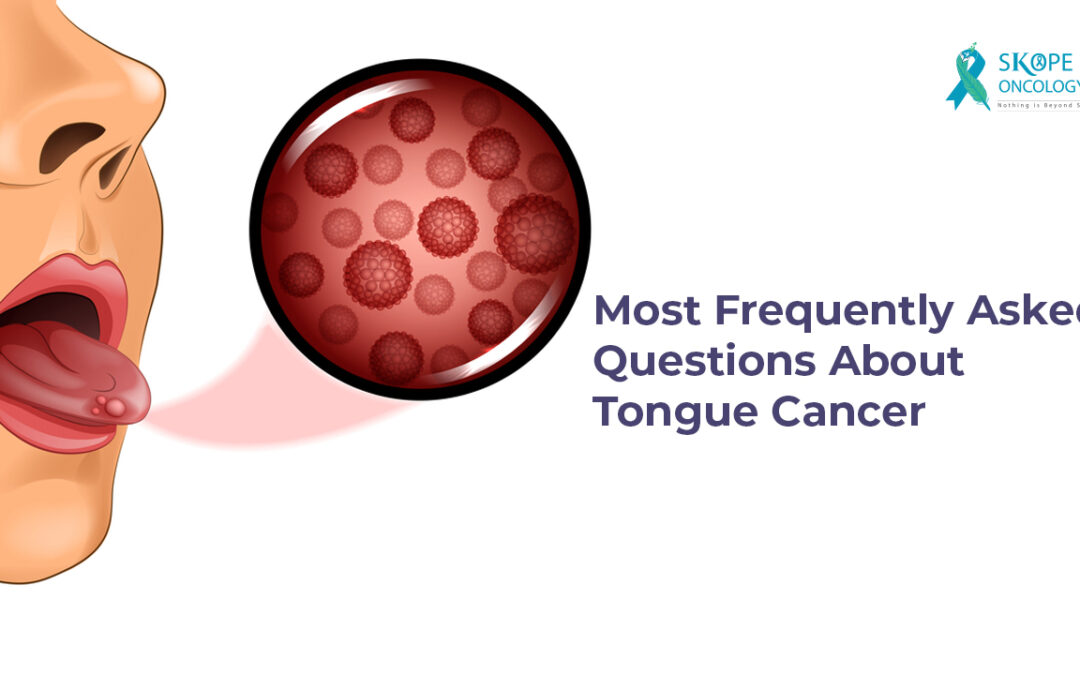
Tongue cancer is a type of head and neck cancer that usually develops in the squamous cells on the surface of the tongue. The symptoms usually include persistent ulcers or sores on the surface of the tongue, pain, and redness, among others.
The following are some of the most frequently asked questions about tongue cancer.
How can I know if I have tongue cancer? What are the early signs?
A painful lump or sore on the side of the tongue that bleeds easily and refuses to heal is one of the early indicators of tongue cancer. Other signs of tongue cancer may include the following:
- Persistent red or white patches on the tongue
- Persistent numbness and soreness in the mouth and throat
- Pain during swallowing
- Burning sensation of the tongue
- A lump in the neck
- Unexplained bleeding from the tongue
If you have any of the above symptoms or are at a higher risk of developing tongue cancer due to one or more risk factors, you should see a doctor and get regular dental check-ups.
Is tongue cancer painful?
Not all symptoms of tongue cancer may be associated with pain. However, pain in the mouth or tongue is a commonly observed symptom. Other painful symptoms include:
- Persistent pain in the mouth
- Speaking, chewing, or swallowing difficulties
- A painful or irritated throat that persists after a few days
- Pain in the neck or ears
- A persistent sensation of something stuck in the throat
Who is at risk of developing tongue cancer?
While anyone can get tongue cancer, some factors have been linked to an increased risk, including:
- Tobacco and alcohol abuse: People who consume large amounts of alcohol and smoke have a 30 times greater risk of developing tongue cancer than those who do not.
- Human papillomavirus (HPV) infection: HPV16 is often linked to oropharyngeal cancers, particularly those in the tonsils and at the base of the tongue.
- Gender: Men are twice as likely as women to have oral and oropharyngeal cancers.
- Age: Oral cancer is most commonly observed in people aged 55 or older.
Genetic conditions: Certain genetic conditions, such as Fanconi anemia and Dyskeratosis congenital (rare conditions that affect the bone marrow), have a very high risk of developing mouth cancer.
How frequently should I get screened for tongue cancer?
Adults over the age of 20 should be screened every three years, and those over the age of 40 should be screened annually.
People with risk factors for mouth cancer, such as tobacco smoking, high alcohol consumption, human papillomavirus (HPV) infection, and/or a family history of cancer, must get an annual oral cancer screening.
Early detection of oral cancer improves your chances of successful treatment. Hence, it is recommended to have regular oral cancer screenings that examine the entire mouth.
Is Tongue Cancer Treatable?
Tongue cancer is curable when detected early. Over time, the tumor may metastasize and spread to other parts of the mouth, other areas of the head and neck, or other parts of the body, and hence can be fatal if not diagnosed and treated promptly.
The treatment option may include any one or a combination of the following:
- Surgery
- Chemotherapy
- Radiation therapy
- Targeted therapy
Do treatments for tongue cancer cause side effects?
Treatments for tongue cancer may cause problems with your speech and difficulty eating and drinking. These could be permanent changes for some people.
Side effects differ from one person to another. However, a few of the most commonly occurring side effects are listed below:
- Fatigue
- Nausea and Vomiting
- Soreness of the mouth and throat
- Difficulty swallowing
- Dry mouth
- Hoarseness of voice
- Altered sense of smell
- Changes in taste
How long do the side effects last?
The duration of side effects from oral cancer treatment varies depending on the stage of the disease and the type of treatment.
Some adverse effects may only last a few weeks or months, while others could last the rest of the patient’s life. If a feeding tube is needed following therapy, it may be removed after the patient is able to eat on his or her own. However, some speech difficulties may remain permanent.